How Coeo Labs is set to breathe life into millions with their indigenous medtech marvels, Saans and VAPCare
From helping newborn babies combat respiratory problems to ensuring patients breathe easy on a ventilator, India’s deep tech startup Coeo Labs is developing indigenous medtech devices to save lives by preventing ‘preventable deaths’.
At St John’s Medical College and Hospital, a large hospital in Bengaluru city, two would-be-entrepreneurs Nitesh K Jangir and Nachiket Deval were participating in a clinical-needs analysis programme run by the InnAccel AIM Fellowship in 2014. The goal of the six-month-long programme was ambitious, albeit simple in its clarity: identify pressing problems in the healthcare industry and build indigenous solutions to address these unmet needs.

(Left to right): Coeo Labs Founders Nachiket Deval and Nitesh K. Jangir with their medtech devices VAPCare and Saans
With that goal in mind, the duo shadowed doctors, patients, nurses, and other hospital staff, dividing their time between the emergency and critical care units to observe any gaps that existed. And they found a slew of gaps that needed addressing, from product level to system- and training-level. Altogether, their findings yielded 120 observations and 70 compelling needs spread across different medical fields, including cardiology and neurology.
Coeo Labs: solving unmet needs of global scale
But these findings aside, it was the many heartwrenching human stories – of lives lost or gravely impacted – that brought the two like-minded innovators together to form their medtech startup Coeo Labs in their mission to create palpable, lasting impact in the healthcare space.
Since its launch in October 2014, these human stories have propelled Nitesh and Nachiket and the Coeo Labs team to build innovative medtech solutions to save precious human lives.
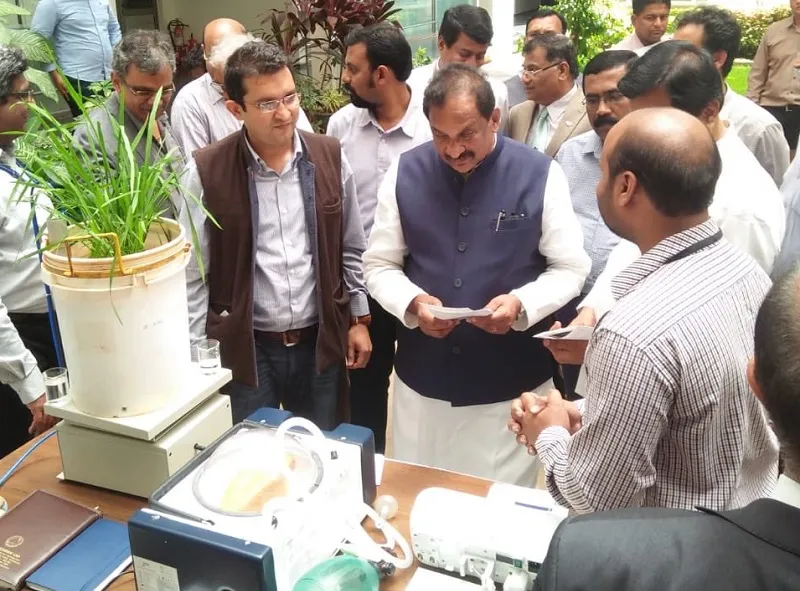
The Coeo Labs team with Dr Taslimarif Saiyed, CEO & Director, C-CAMP, at an exhibit at C-CAMP for Saans and VAPCare
Backed by InnAccel, Biotechnology Industry Research Assistance Council (BIRAC), C-Camp, and Department of Biotechnology, among others, the two entrepreneurs have, for the past four years, been on a quest to address unmet needs in the healthcare industry by engineering innovative, high-quality medtech devices for not just the Indian market but across the globe.
For the two unassuming entrepreneurs, two such ‘heartbreaking’ stories highlighted the urgent need to develop Saans, a low-cost, portable breathing support device for babies with respiratory problems, and another critical care device VAPCare, which prevents the risk of ventilator associated pneumonia, a common cause of death in patients on long-term ventilator care.
Need for Saans and VAPCare
While at St John’s Hospital, the duo saw a family bring in a newborn baby, from another smaller hospital, in an autorickshaw. The baby, who was suffering from a common respiratory problem called respiratory distress syndrome (RDS), was being transferred to the tertiary care hospital, but with no medical infrastructure to support the baby’s breathing during the transfer, the parents lost the baby before doctors at the bigger hospital could treat him.
“That was really heartbreaking for us because we knew solutions exist. But these solutions are not always in places where they are really needed,” says Nitesh, an electronics engineer from the Gyan Ganga College of Technology in Jabalpur.

A newborn baby receives breathing support through Saans in a semi-urban hospital in Bengaluru
“Not all hospitals have neo-natal ICUs or the infrastructure to provide breathing support. And yet, most of the births happen outside centres that have such infrastructure. In fact, about 70 percent of all births in India happen in places where there is no access to neo-natal ICUs,” he adds.
At the same hospital, they also saw how a man, who was recovering from a head injury, had contracted infections while on long-term ventilator care, worsening his condition despite initially being on the path of recovery.
“He was in the ICU on a ventilator and was supposed to be out of the ICU within two days. But even after two days he was still there and we found out that had developed pneumonia and this is what shocked us. Because we always considered hospitals to be places where people get cured and not where they get more infections,” Nachiket says.

A critical care patient on VAPCare
When Nachiket and Nitesh did a deep dive into the problem, they found that ventilator associated pneumonia was a common global problem that needed to be addressed. In India alone, 6,00,000 patients get Ventilator Associated Pneumonia (VAP) each year, with the mortality associated with this condition as high as 40 percent.
With respiratory distress syndrome (RDS) too, research showed that in India alone, more than 162,000 babies die every year, of which over 30 percent deaths occur due to the lack of infrastructure during transportation to tertiary care hospitals.

A newborn baby at a semi-urban hospital in Bengaluru on breathing support through Saans
They also found that a stand-alone Continuous Positive Airway Pressure (CPAP) device, which is used to help babies with RDS, costs more than Rs 150,000, making it unaffordable to stock such devices at primary and rural care centres.
CPAP, a technology recommended by the World Health Organisation, enables the provision of constant pressure and air flow to babies to prevent their alveoli, which is an important part of the respiratory system, from collapsing, thus ensuring their lungs remain open.
“India has one of the highest rates of respiratory distress syndrome, which requires immediate breathing support. If babies don’t get immediate breathing support there are chances of brain injury, developmental issues and high chance of death due to lack of oxygen to the brain,” says Nitesh.
The risk of a premature babies suffering from respiratory distress syndrome is also dramatically higher, with studies showing that over 60 percent of them develop this condition. Studies also indicate that over 1.1 million babies, of the nearly 15 million babies born prematurely every year, die due to respiratory distress syndrome.
Saans: a novel, indigenous solution to help babies breathe easy
This led Nachiket and Nitesh to participate in the medical hackathon organised by CAMtech India and GE Healthcare in 2014. There, they met a doctor, Data Santorino from MUST Uganda, who pitched the same problem during the event and recounted similar problems they faced in Africa, and together, the three and Dr Kristian Olson, a professor at Harvard Medical School and director of CAMTech, and Dr Jagdish Chaturvedi, came up with the idea to build Saans.
And the foundation they sought to build their product on was simple: provide a breathing support system that does not have any dependency, whether it’s on physical infrastructure or on the availability of a trained clinical person. They were also clear that the breathing support or CPAP device they build should be gold standard quality, low cost, and be applicable for use across the globe.
Today, Coeo Labs’ Saans, which in Hindi means “breath” or “air,” does refreshingly what the name itself suggests: give life to babies suffering from respiratory problems.
Designed and built by a team of engineers, doctors, and product designers at Coeo Labs, the device was part of the Nitesh and Nachiket’s aim to engineer indigenous, affordable healthcare solutions that have the potential for high impact and mass reach.
“Resourcing, getting the right materials also ensured that we could bring down the costs. So, our CPAP is one third the cost the multinational CPAPs available in the market,” Nachiket says.
But the USP of Saans is not just its cost. The Coeo Labs team has designed Saans as the world’s only neo-natal mechanical CPAP device that can work with or without electricity, as it has an inbuilt battery backup. The simple-to-use, portable device can also work when oxygen is available, or operated manually by pumping air like a regular air pump.
What’s key is that Saans can convert variable air pressure into a constant air flow that is needed for a baby with RDS. Plus, it’s designed to ensure it’s simple enough for the parents or relatives to use the device, without any formal training in situations where a healthcare worker is not available to give CPAP.
“Our idea was that across the globe, specifically in developing countries, we don’t want any case where we are unable to save a baby because of the lack of a device that can provide breathing support. So, we don’t want them to die because of lack of availability of devices or training or technological solutions. That’s the whole idea. We don’t want these cases to happen anymore,” says Nitesh.
And that’s exactly what Saans has successfully achieved in the three hospitals – one urban, one semi-urban and one rural – where this device is currently being used to provide care in low resource settings.
Dr. Jagadish, a pediatrician at MGV Hospital, a rural tertiary care hospital, in Hoskote, Bengaluru, says,
“For us when we have such a large load of babies, most of our devices are always full. So Saans, which is a low-cost device, can be used for many of those babies who cannot afford a higher-cost device and who can be helped both during transport from a rural peripheral centre to our hospital and in our hospital."
He adds that more than 40 babies have reaped the benefits of this device in the past six months.
Saans, which is now ready for commercial use, has completed a clinical evaluation on 50 neonates and achieved success in delivering CPAP from this device.
VAPCare: a first-of-its-kind medtech device
Coeo Labs’ VAPCare device, which was a project funded by BIRAC, is also the first-of-its-kind intelligent secretion management and oral hygiene system that reduces the risk of ventilator associated infections for patients in critical care.

Coeo Labs Founders Nachiket and Nitesh at the nationwide launch of VAPCare in Delhi
Until recently, infections in patients on ventilator, called aspiration pneumonia, was considered a ‘drug problem’, which could be treated by giving antibiotics.
“When we studied VAP, we understood that it is a hard-core engineering problem where saliva and secretions accumulate and go inside the lungs, and that’s where we took an engineering approach where the most logical solution was to make sure that none of these secretions roll down, and remove it from multiple locations,” says Nitesh.
Research shows that aspiration of infectious bacteria present in the oropharynx, the area behind the mouth that is in the middle part of the throat, and the gastrointestinal or digestive tract is the main cause of ventilator associated pneumonia.
“Till now, even in the medtech device sector, everyone was more focused on removing secretions from one location, which is the subglottic area, below our vocal chords. Ours is the only device which can remove secretions from multiple locations,” Nitesh says.
VAPCare uses artificial intelligence and sensor-based technology to manage secretions and oral hygiene in three locations: the oral cavity, the oropharayngeal, and the subglottic areas. In doing so, it ensures these secretions do not reach the lungs and cause infections. VAPCare’s unique sensor-based technology detects the presence of secretions and ensures no suctioning is done in the absence of secretions so as to avoid any injuries.
Watch this video to understand how VAPCare works.
This makes VAPCare the only device that can auto-detect secretions and automatically push in mouthwash and remove the fluid regularly, thus doing away with dependencies on healthcare workers. In addition, VAPCare is compatible with all ventilator machines and is non-invasive.
VAPCare, which has been used in nine hospitals across multiple states in India, has been effective so far in preventing the onset of ventilator associated infections for patients using the device. The device, which is in commercial stage, has been granted patents in the US, China, and India, receiving widespread appreciation and interest from doctors in different markets.
“It is a tremendous feeling of joy and happiness to see that doctors are appreciating your work and that it’s actually saving lives. So, we have got patients who because of the device have been treated properly, the secretions have been managed well, because of which they haven’t contracted VAP. And that is a very fulfilling feeling you get after all the effort that you have put in,” says Nachiket.
Looking ahead
And yet, Nachiket, Nitesh and their team at Coeo are only just getting started in their journey to save millions of lives through VAPCare and Saans.
The Coeo team will be running pilot programmes for Saans in multiple states across India, wherein each state that uses this device, generates data on its impact, which is ultimately made available to the government for deployment across all healthcare centers. The aim is deploy Saans at both public and private healthcare centres, as many small nursing homes in tier I cities also do not provide this kind of CPAP facility.
“First we want to work with the government, and not just with primary healthcare centres but also small-scale birth centres/nursing homes. Our ultimate goal is that every healthcare centre in India, where child deliveries happen, should have this device.” Nitesh says.
To put it simply, Coeo Labs has made it its mission to breathe life into every newborn through Saans, and to other patients through its other medtech inventions such as VAPCare.
As Nachiket poignantly says,
“The next big thing for Coeo Labs would be to scale up. Taking our devices to all possible patients, all the people for whom this would have an impact. In short, to take it to the masses and to ensure that there is impact because of what we are doing.”