COVID-19 vaccinations: What's the progress?
How many people have been vaccinated? Which vaccines are approved? Here's the global progress on vaccination against SARS-CoV-2, the virus that causes COVID-19.
There are more than 50 clinical trials worldwide testing potential vaccines, known as candidates, against COVID-19. So far, four of the vaccine candidates have been approved.
The approved vaccines were developed by:
Still, the majority of vaccine candidates for COVID-19 are still in a preclinical phase. That means the candidate vaccines are being tested in animal experiments, for example, rather than with human patients.
When those tests are deemed successful, candidate vaccines can move into clinical trial phases. That's when they are tested with humans. There are three clinical trial phases for efficacy and safety before a vaccine can be approved for use by humans. The phases differ from each other, most significantly in their scale:
- In Phase I, a vaccine is tested on small patient groups.
- In Phase II, a vaccine is tested on larger groups of at least 100 patients; researchers can also test their candidate vaccine in specific subgroups, such as people with preexisting conditions, or patients with particular demographic characteristics, such as a higher age group.
- In Phase III, a vaccine candidate is tested on at least 1,000 patients.
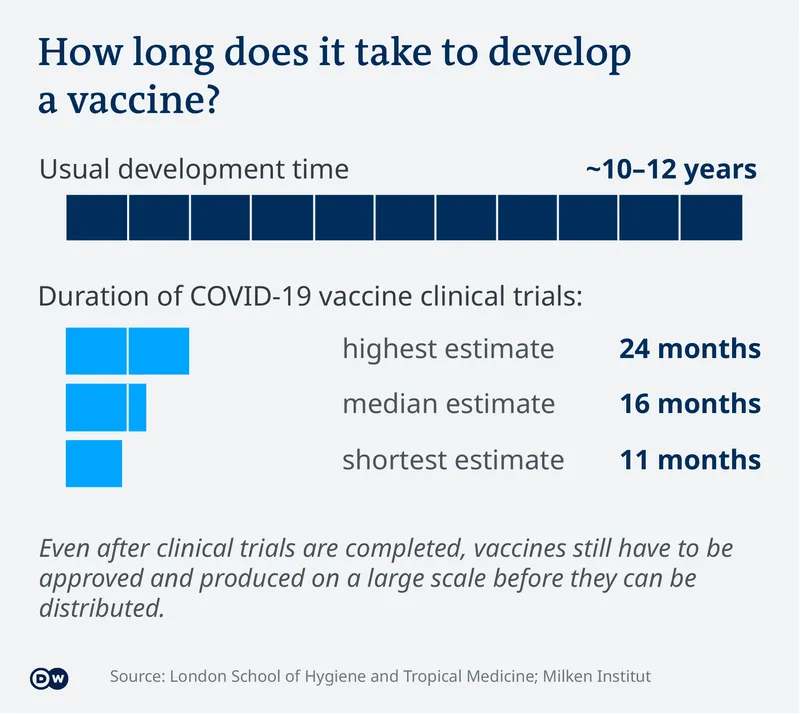
Image credit : Deutsche Welle
Some companies, such as BioNTech-Pfizer in Europe, and Sinovac in China, have tested their vaccine candidates in several trials in parallel. For example, they have tested the same vaccine but in different age groups or with different dosages.
If clinical trials are successful, a company can formally apply to regulatory bodies to have their vaccine approved for use by the general public.
Three regulatory authorities are considered to be particularly important in this context: The FDA in the US, the European EMA, and the Pharmaceuticals and Medical Device Agency in Japan.
What happens after a vaccine has been approved?
When a vaccine is approved, it doesn't mean everybody can get it immediately.
First, the vaccine has to be produced on a mass scale. With COVID-19, manufacturers aim to produce billions of doses by the end of 2021.
Second, logistics experts have to ensure appropriate distribution of the vaccine, and political leaders have to decide who gets the vaccine first.
In the end, though, it will be up to each individual to decide. A 2020 survey of more than 13,000 people in 35 countries most affected by COVID-19 showed that the majority of people asked would choose to get vaccinated.
A survey by YouGov in January found that the willingness to be vaccinated increased in some European countries, whereas the trend isn't as clear in other regions of the world.
How fast can vaccines be developed?
It can take several years to develop an effective and safe vaccine. On average, it takes between 10 and 12 years, but it can take longer. The search for a vaccine against HIV has been going since the early 1980s — so far without success.
In the case of COVID-19, researchers are racing to shorten the time it usually takes because of the ongoing pandemic. Despite the pressure that that brings, vaccine developers, manufacturers and the World Health Organization (WHO) say there will be no compromises on safety.
Research teams are aiming to accelerate, or limit, the time it takes to get to approval during the pandemic to an average duration of 16 months.
That will only be the beginning. Once clinical trials are successfully completed and a vaccine is approved and produced, researchers start phase IV, during which they observe the progress of vaccinated patients.
Which types of COVID-19 vaccine are in development?
Researchers are pursuing 13 different approaches for vaccines against COVID-19.
Most of the vaccine candidates use a protein-based subunit — so, instead of using a complete pathogenic virus, they are built on a small component of it, such as a protein found in its outer shell.
That protein is administered to patients in a high dose, with the aim of inducing a fast and strong reaction by the human immune system.
The hope is that the immune system will "remember" the protein and trigger a similar defense reaction if or when it comes into contact with the actual virus.
Vaccines against hepatitis B and HPV (human papillomavirus), for example, are based on this principle.
Four additional approaches have made it to phase III.
Nonreplicating viral vectors are a type of so-called recombinant vaccines: Researchers modify the virus's genetic information by switching on or off or altering certain functions. By doing that they can, for example, reduce the infectiousness of a virus. Such genetic modifications, however, require that science already has detailed knowledge about which parts of a virus' genetic material are responsible for which functions in order for them to be able to manipulate them effectively. The term "nonreplicating" means that the virus in the vaccine enters cells in the human body but is unable to reproduce there on its own.
Inactivated vaccines use a "dead" version of the pathogen. They tend to provide a lower level of protection than live vaccines. Some vaccines in this class have to be administered several times to achieve sufficient immunity. Examples of inactivated vaccines include ones against influenza and hepatitis A.
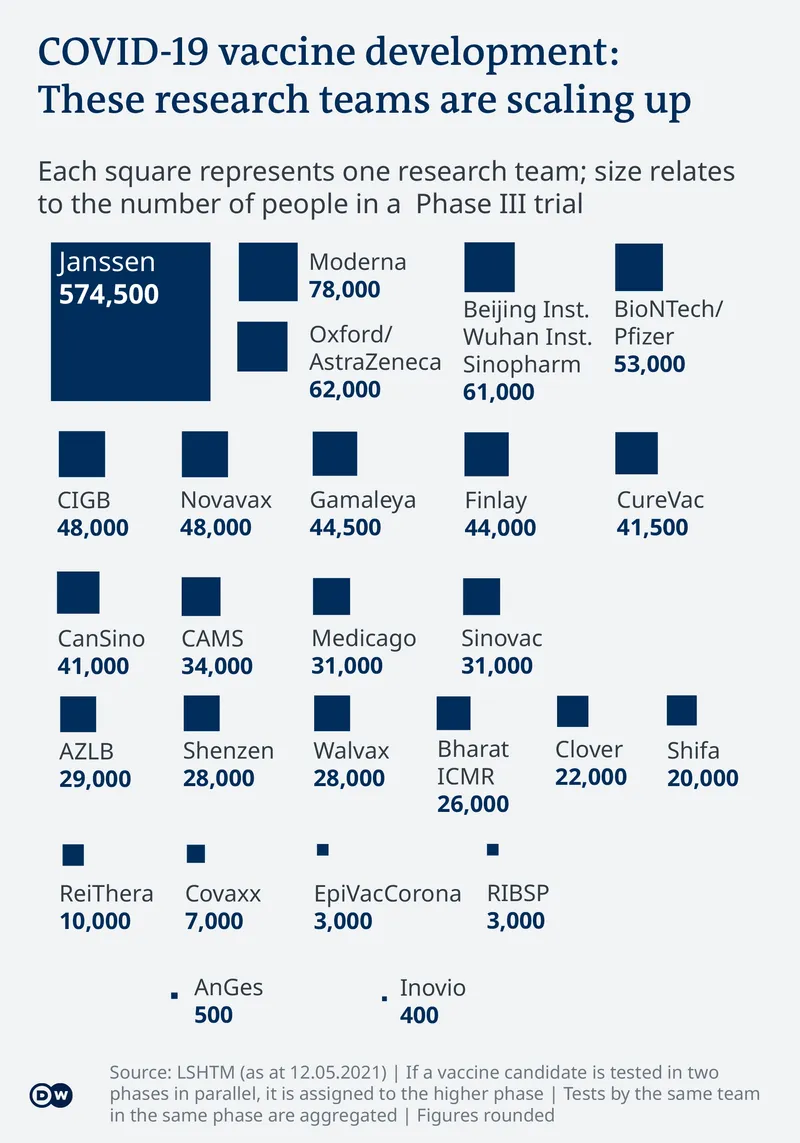
Image credit: Deutsche Welle
RNA vaccines follow a different strategy, without using any "real" component of the virus at all. Instead, researchers aim to trick the human body into producing a specific virus component on its own. Since only this specific component is built, no complete virus can assemble itself. Nevertheless, the immune system learns to recognize the non-human components and trigger a defense reaction.
Vaccines based on viruslike particles use another approach: Researchers only use the empty virus envelope — without any genetic material inside of it — to train the immune system.
With DNA-based vaccines, patients are injected with the virus's genetic makeup for the human body to produce virus particles itself without being actually infected. Confronted with these self-produced virus particles, the immune system is supposed to learn to recognize and fight the actual virus.
Who is working on a COVID-19 vaccine?
At time of writing, there were well over 100 research teams worldwide developing a COVID-19 vaccine. So far, 26 teams have advanced their vaccines to the third phase of clinical trials. Although some of these vaccines have already been approved in some countries, they still continue to be tested in clinical trials in parallel.
Five teams stand out for conducting the most extensive clinical trials:
- Belgian company Janssen Pharmaceutical is testing its candidate vaccine, which is based on a non-replicating viral vector, on about 574,500 people in South Africa, Belgium, the United States, Argentina, Brazil and Colombia.
- The US company Moderna is testing its RNA-based vaccine on 78,000 people in the US, Canada, France and Japan
- In a public-private partnership between the University of Oxford and the British company AstraZeneca, researchers are testing their vaccine candidate on approximately 62,000 people in the US, Chile, Peru and the UK. Their vaccine is based on a similar principle to Janssen's.
- The Chinese company Sinopharm is working in various constellations with the Beijing Institute and Wuhan Institute. Taking all trial series together, they are testing an "inactivated" vaccine on around 61,000 people in Bahrain, Jordan, Egypt, Morocco, Argentina and Peru.
- A German company, BioNTech, is pursuing a different approach: It is focusing on RNA-based technology and testing the BioNTech-Pfizer candidate vaccine on about 53,000 people in the US, Argentina and Brazil, among other countries.
(This article by author Gianna-Carina Grün was originally published on Deutsche Welle.)
Edited by Anju Narayanan
(Disclaimer: The views and opinions expressed in this article are those of the author and do not necessarily reflect the views of YourStory.)