Working on frontlines to treat COVID-19 has been exceptionally challenging, says MSF’s Nimrat Kaur
Dr Nimrat Kaur, Regional Deputy Project Coordinator, Asia at Médecins Sans Frontières (Doctors Without Borders) is working on the frontlines at the COVID care centre in Patna, Bihar.
It's been a little over six months since the world first started taking note of the coronavirus spreading through provinces in China and other countries.
Today, it’s a global pandemic affecting almost all nations in the world and the fight against the virus has seen heightened efforts around the globe to come up with new treatments, a vaccine and hopefully, a cure.
In India, the coronavirus curve has seen an upward spike since the reopening of the economy under Unlock 1.0. According to the Ministry of Health and Family Welfare, active cases in the country stand at 2,69,789 with recoveries at 4,76,377 as on July 9, 8am.
The medical fraternity is on the frontlines taking care of COVID positive patients, testing, conducting research and also risking their lives in the process.
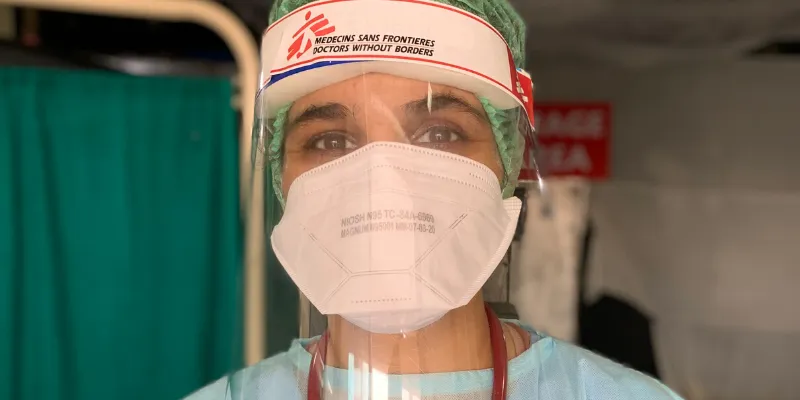
Dr Nimrat Kaur is one of the doctors on the frontline fighting against the pandemic.
HerStory spoke to one such frontline doctor, Dr Nimrat Kaur, who is the Regional Deputy Project Coordinator, Asia at Médecins Sans Frontières (Doctors Without Borders) and is currently based in Patna, Bihar at MSF’s 100 bed COVID-19 treatment centre for patients with mild and moderate symptoms.
In a conversation with HerStory, Nimrat talks about her work on the frontlines, the toll it takes on medical personnel, challenges, and more.
Here are edited excerpts:
HerStory (HS): Being on the frontlines of a global pandemic is not easy, how do you prepare yourself?
Nimrat Kaur (NK): When I heard about the opportunity to volunteer as a medical doctor in Patna, my first instinct was: I trained for this and I want to be on the frontline for this. This is probably never going to happen again in my career. I think for most medical staff, this personal dilemma of wanting to help at the cost of risking their own lives is the biggest struggle. We all are living away from our families and they also get scared and anxious. We are trained to manage the illness, but these are unprecedented times and literally no one was prepared for something like this. I think each day is a new learning experience where we face new challenges and learn to cope with them. But at the same time, it is unfortunate to see how frontline workers are being discriminated against by some in these difficult times. That's extremely disheartening because frontline workers are working to the bone to save lives.
HS: Can you describe a day in your life…
NK: It’s a typically a long and tiring day for anyone working on the frontline. The staff working inside the hospital usually has 12-hour long shifts. My day usually starts with a quick early morning workout to prepare myself not just physically but also mentally for another long challenging day. I get ready and walk to the facility. I change into my scrubs and PPE and enter the ward where we take our usual rounds.
In a 12-hour shift we try to squeeze in at least half an hour break each to get out of the PPE and breathe a little or use the washroom and of course, eat.
HS: What kind of challenges are you facing while dealing with the pandemic?
NK: As medical staff, we are trained to manage illnesses but working on frontlines to treat COVID-19 has been exceptionally challenging. There is a huge element of your own safety and mental health involved. While we are treating patients, we try our best to stay safe and that requires being in PPEs during our shifts, minimising our physical and social interactions outside of work as part of infection control - all these cause more anxiety and fear than the actual management of the virus.
It is also physically exhausting as wearing PPEs, which includes gloves, face masks, face shield, coveralls, shoe covers, hairnet, etc, for 12 hours is not easy, especially in Patna’s hot weather. We get rashes on the face and constant pressure induced headaches because of the face shield. We also have to keep on motivating each other round the clock to push through these difficult times.
For instance, each time someone steps out of the hospital to use the washroom, the PPE gets contaminated and needs to be changed. But this is not possible as PPEs are expensive and are in limited supply. So, we try to limit our washroom visits by not drinking enough water or eating less. We are mostly soaked in sweat because it is very suffocating.

Dr Nimrat Kaur all clad in PPE and at work in the COVID-19 treatment centre in Patna, Bihar.
HS: What kind of shortfalls has the pandemic exposed in India’s healthcare system?
NK: I personally believe that with this pandemic, we have all realised the importance of strengthening our public healthcare infrastructure. So far, we have seen that the maximum of the cases this virus has seen, can be managed in a low resource setting healthcare facility. We have a huge number of primary healthcare centres across the nation that could have been utilised in managing many of the cases that we are now seeing across rural India.
HS: When and how do you think the pandemic will come to an end?
NK: The new normal is reduced physical interaction, increased levels of infection prevention control and working under severe stress. The only preventative things people can do in these environments is to regularly wash hands, cough into elbows, avoid spitting and if they feel unwell, try to keep some distance from others - especially older people or those who suffer from other illnesses.
It is also essential for people to pay extra attention to their mental health. These are tough times and we all need support. Be close to your loved ones and try to share your feelings with people you trust. Things will get worse before they get better, so we have to collectively go through this phase and move on.
Edited by Rekha Balakrishnan